Chronic conditions: A closer look at a primary driver for quality reporting
I recently thought back to a conversation I had many years ago with close colleagues about the health conditions of our parents. High blood pressure and obesity were the top diagnoses affecting our families, but that was 15 years ago when our parents were in their mid-forties. Fast forward to today, when they’re now in their 60’s, and the likely diagnoses affecting our parents include diabetes, cancer, stroke and heart disease. Chances are many of your patients are like our parents, afflicted by one or more chronic diseases. As of 2012, almost one in two adults in the U.S., about 117 million, suffer from at least one chronic condition and almost one in three adults have two or more chronic conditions.1,2 The simplicity of that original conversation has been replaced by a much more complex scenario. This is true for many of us on a personal level, but also much more broadly.
Chronic conditions, as defined by the U.S. National Center for Health Statistics, are conditions that last three months or longer. Chronic conditions are generally incurable, require ongoing medical attention, and are the leading cause of death and disability in the United States.1 The prevalence of chronic conditions increases with age. 80% of people 65 years and older have multiple chronic conditions. Chronic conditions are responsible for 7 out of 10 deaths, with heart disease and cancer accounting for almost 48% of all deaths.2 Among medicare beneficiaries, high blood pressure, high cholesterol, heart disease, arthritis and diabetes are the most common chronic conditions.3
Percentage of Medicare beneficiaries with the 15 selected chronic conditions: 2010
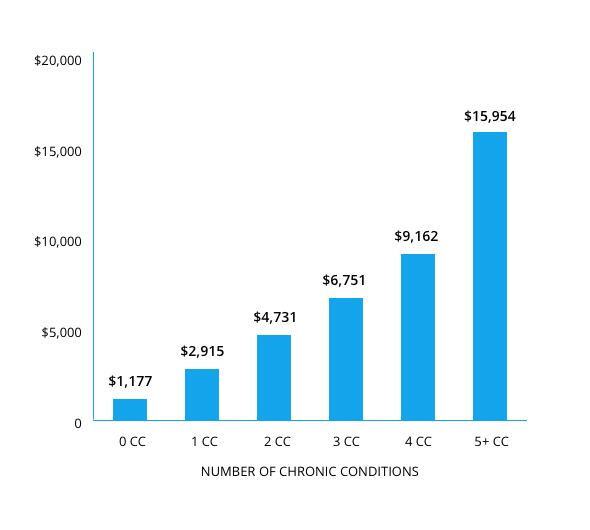
Chronic conditions are costly to treat
Although chronic conditions are often preventable and manageable if detected early, once they develop they are generally incurable and require constant monitoring and treatment. This contributes greatly to health care costs. According to the AHRQ-sponsored 2010 Medical Expenditure Panel Survey, 5% of the population account for 50% of overall healthcare expenditures, with treatment for patients with one or more chronic conditions accounting for 86% of all healthcare spending.4
Average healthcare spending per capita, by number of chronic conditions: 2010
Evidence-based quality reporting for chronic diseases exists across healthcare
The widespread prevalence of chronic conditions and the corresponding dramatic increase in national spending to manage them is a primary driver for the quality reporting on chronic conditions across health care. Not only are physicians increasingly reporting quality measures on chronic conditions, but also hospitals, nonprofits, for-profits, and government agencies.
Healthcare segments that report on quality measures for chronic disease
| Healthcare segment | Examples |
|---|---|
| Providers | Eligible clinicians participating in the proposed Quality Payment Program |
| Eligible providers participating in Meaningful Use Stage 3 | |
| Non-profit organizations | National Committee for Quality Assurance (website) |
| The Joint Commission (website) | |
| For-profit companies | Healthgrades (website) |
| Payers participating in HEDIS (website) | |
| Government agencies | Centers for Medicare and Medicaid services (website) |
| Agency for healthcare research and quality (website) |
Quality measures will continue to evolve
While we continue to work on tackling the growing epidemic of chronic diseases, significant gaps still remain in quality metrics, both specific to chronic conditions and quality measurement more broadly:
1. The definition of “quality” varies across patients, physicians and payers. Although there are multiple organizations developing quality measures, most of them focus on process and structure measures while pushing outcome measures to the sidelines.
2. Not having a single source of standardized clinical quality measures (CQMs) has been an Achilles heel for quality measurement. As a step in the right direction, the Affordable care act tasked CMS and AHRQ with the development of a standardized core set of health quality measures for Medicaid eligible adults. The core set includes measures form NCQA HEDIS, JCHACO, and CMS.<sup>5</sup>
3. Most of the CQMs developed by various organizations focus mainly on only a subset of major chronic conditions. A survey by Avalere shows that commonly occurring cancers such as prostate cancer and mental health measures, such as depression are highly underrepresented in the medicare pay-for-quality programs.<sup>6</sup> One of the other major gaps that exists is the fact that most quality metrics are single disease specific and do not take into the fact that of patients suffering from chronic conditions, one in three has multiple chronic conditions (MCCs). With MCCs accounting for almost all Medicare hospital readmissions, it is becoming increasingly common for physicians to treat patients with MCCs. However, applying single disease guidelines to patients invariably increases the risk of poor outcomes.<sup>3</sup>
Needless to say, there is an urgent need for the next generation of quality measures to focus on the most commonly occurring chronic condition clusters in order to promote better care coordination and management for patients and help them enjoy a better quality of life.
Your EHR can help you manage chronic conditions and participate in quality reporting
One of the things we’re passionate about at Practice Fusion is helping your practice stay on the leading edge of care, including in the management of chronic conditions. Your certified EHR from Practice Fusion helps you track the health of your patients with chronic conditions and can proactively notify you when a patient may be at risk for select conditions through clinical decision support (CDS). CDS advisories allow you to learn more about your patients so you can better manage their chronic conditions. The time spent hunting through the chart for the last diabetic eye or foot exam can be better used getting to know about the patient’s individual needs. For example, CDS advisories in Practice Fusion’s EHR will let you know when it’s time for your patient’s diabetic eye or foot exam based on consensus guidelines — and in certain cases, when to check the Hgb A1c.
These CDS advisories, along with automatic dashboards, can also help you participate in current quality reporting programs and the proposed Quality Payment Program (QPP) coming in 2017. For example, the Physician Quality Reporting System (PQRS) dashboard in your EHR helps you automatically monitor your progress on your Clinical Quality Measures (CQMs) and report them when you’re ready.
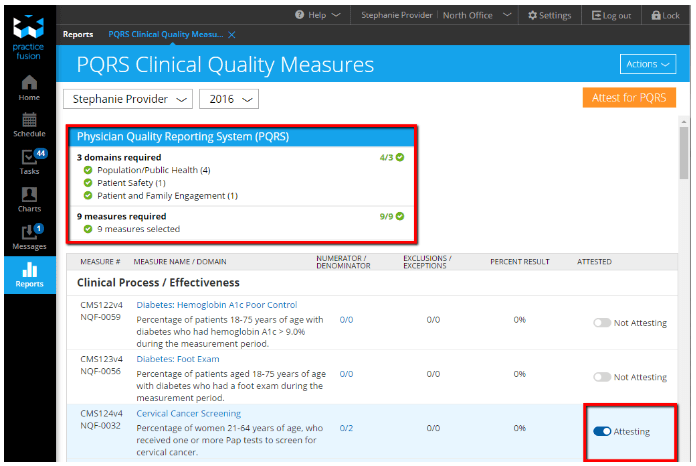
As the requirements for the QPP are finalized by CMS, we’ll be updating your EHR to help you participate in the new program.
Don’t have an EHR from Practice Fusion? If you’d like to see everything our EHR can do for your practice, try it out. It takes less than 5 minutes to sign up and start charting.
References:
- Centers for Disease Control, Chronic Disease Overview, available at: https://www.cdc.gov/chronicdisease/overview/. Accessed July 2016.
- Agency for Healthcare Research & Quality, Multiple Chronic Conditions Chartbook, available at: https://www.ahrq.gov/sites/default/files/wysiwyg/professionals/prevention-chronic-care/decision/mcc/mccchartbook.pdf. Accessed July 2016.
- Centers for Disease Control and Prevention, NCHS Obesity Data, available at: https://www.cdc.gov/nchs/data/factsheets/factsheet_obesity.htm. Accessed July 2016.
- Centers for Medicaid and Medicare services, Chronic conditions amoung medicare beneficiaries, available at: https://www.cms.gov/research-statistics-data-and-systems/statistics-trends-and-reports/chronic-conditions/downloads/2012chartbook.pdf. Accessed July 2016.
- Federal Register, Medicaid Program: Initial Core Set of Health Care Quality Measures for Medicaid-Eligible Adults, available at: https://www.federalregister.gov/articles/2012/01/04/2011-33756/medicaid-program-initial-core-set-of-health-care-quality-measures-for-medicaid-eligible-adults#h-6 Accessed July 2016.
- Avalere, Lack of Quality Measures for Cancers and Other Serious Diseases Limits Medicare’s Ability to Pay for Value, available at: https://avalere.com/expertise/life-sciences/insights/lack-of-quality-measures-for-cancers-and-other-serious-diseases-limits-medi/. Accessed July 2016.



