December 21, 2023
Be Prepared for MIPS PY 2023: Four Steps to Pain-Free Reporting

The Merit-Based Incentive Payment System (MIPS) was designed to tie Medicare payments to quality and cost-effective care, to drive improvement in care processes and health outcomes; increase the use of healthcare information; and reduce healthcare costs. Data are collected in 4 performance categories and used to calculate a final MIPS score:
- Quality
- Promoting Interoperability
- Improvement Activities
- Cost
The Centers for Medicare & Medicaid Services’ (CMS) Quality Payment Program (QPP) collects and calculates data for cost measures; the clinician or practice collects and submits data for the other 3 categories.
The MIPS 2023 Performance Year (PY) extends from January 1, 2023 through December 31, 2023, and MIPS-eligible clinicians are required to report PY 2023 data by March 31, 2024. MIPS-eligible clinicians will then receive payment adjustments based on the MIPS final score calculated from data submitted (or not submitted) for services provided. MIPS PY 2023 payment adjustments will be applied to Medicare Part B claims from January 1 through December 31, 2025.
As the MIPS PY 2023 draws to a close, it’s critical to ensure all the puzzle pieces are in place to streamline your MIPS participation. In this article, we have assembled 4 steps that will streamline the process for all MIPS-eligible clinicians, plus resources to help you complete your preparations for submitting MIPS PY 2023 data.
Review MIPS eligibility
To participate in MIPS, you must ascertain that you’re meeting all the requirements established by CMS and the QPP. As a first step, reviewing your MIPS eligibility is crucial, as eligibility requirements change every year. The QPP provides the QPP Participation Status Tool where, by entering your National Provider Identifier (NPI) number and Taxpayer Identification Number (TIN), you can learn whether you are eligible for MIPS participation—and whether you are required to participate. Additional information about 2023 MIPS eligibility requirements can be found on the QPP website.
If you are participating in MIPS as a small practice, please review the small practice eligibility requirements to confirm your practice meets CMS specifications for a small practice. The QPP also provides numerous resources specifically addressing small practice eligibility and participation in MIPS, including:
- The QPP website (a centralized location for resources)
- The Small Practices page of the QPP website
- The QPP Webinar Library
- The QPP Resource Library
- The Explore Measures & Activities tool to help identify practice-relevant measures and improvement activities
- 2023 Small Practice Eligibility and Participation FAQs
If you haven’t already, you will also need to register for the QPP with CMS prior to your MIPS submission.
Set up your MIPS Dashboard
Practice Fusion’s MIPS Dashboard is an easy-to-manage tool that enables you to track your progress in the 3 performance categories for which CMS requires data tracking and submission. All users participating in the MIPS program should set up individual MIPS Dashboards in Practice Fusion. Note: If you are submitting for a group, please make sure to set up the group dashboard prior to the end of the reporting period (before January 1, 2024.)
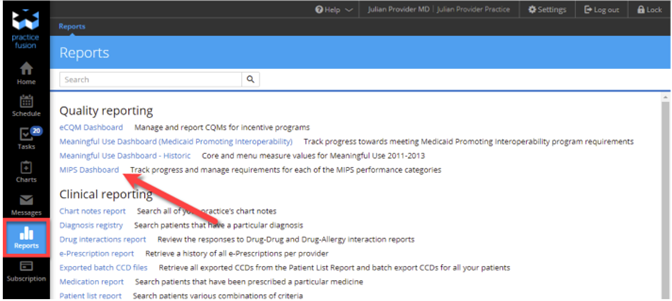
You can access the MIPS Dashboard from the Reports section of the Practice Fusion EHR. Click MIPS Dashboard under the Quality Reporting section.
Select your name and the current PY to set up your individual MIPS Dashboard, then click Set up your reporting periods or the MIPS Settings link. (If setting up any of the PY Quality reporting dashboards for the first time, you will need to opt in to run performance calculations.) Select the desired reporting period and click Save. Note: Data may take up to 48 hours to display.
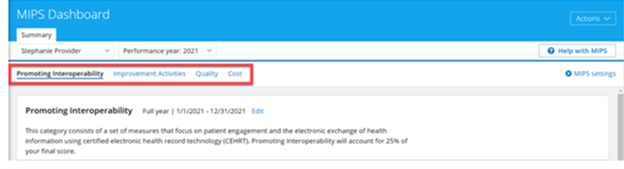
The Dashboard is separated into 4 sections for the 4 MIPS performance categories.
Promoting Interoperability (PI)
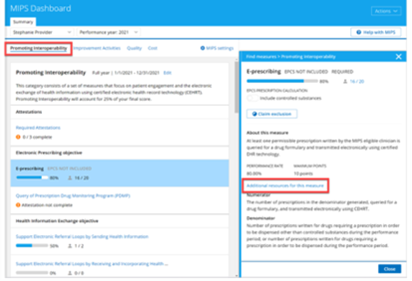
You can access available PI measures, including required attestations, on the Promoting Interoperability card. Clicking an individual PI measure will provide a description of the measure, or you can click the Additional resources for this measure link in the measure description for more detailed information.
Improvement Activities
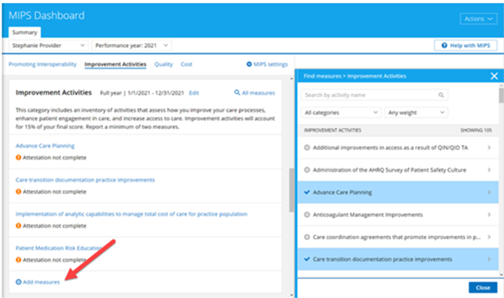
There is no limit to the number of improvement activities that can be tracked. To begin tracking, click Add measures from the Improvement Activities card, then use filters at the top of the list to search for specific improvement activities. Once you’ve located a desired activity, click Save to Dashboard to start tracking.
Quality
Click Add measures from the Quality card to view a list of the electronic Clinical Quality Measures (eCQMs) that Practice Fusion supports for the current PY. Select a specific item from the list to view measure details and your current measure score. You can also access suggested item workflows by clicking the Learn more about completing this measure links within each description.
To start tracking a measure, click Save to Dashboard.
Note: The quality measure “Medical Attention for Nephropathy” is no longer eligible for MIPS 2023 and is no longer supported in Practice Fusion.
Cost
The Cost card only contains information about the category. Since Medicare calculates your Cost performance category score using claims data, you are not required to submit additional data for this category.
Pull QRDA files before March 31, 2024, deadline
MIPS-eligible clinicians are required to report all data collected during the MIPS PY 2023 by March 31, 2024.
The Quality Reporting Document Architecture (QRDA) is a document standard based on HL7 Clinical Document Architecture, which can be used to share quality measure data electronically. With QRDA, providers and practices can report quality measure results in a structured, consistent format and can securely exchange eCQM data between systems.
Two types of QRDA files can be generated using the Practice Fusion EHR:
- QRDA Category I (QRDA I): This file type is a report on the level of the individual patient. It contains quality data for 1 patient for 1 or more eCQMs.
- QRDA Category III (QRDA III): This file type is an aggregate quality report containing quality data for a set of patients for 1 or more eCQMs, PI measures, and/or Improvement Activities.
MIPS-eligible clinicians can participate as individuals, as part of a group, or both.
Individual report generation
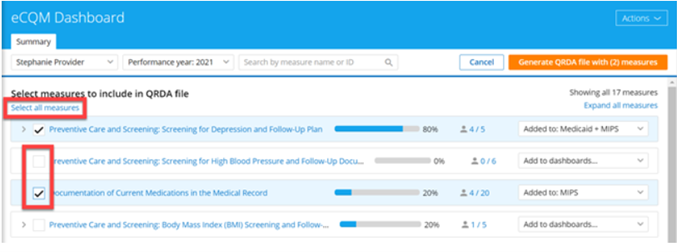
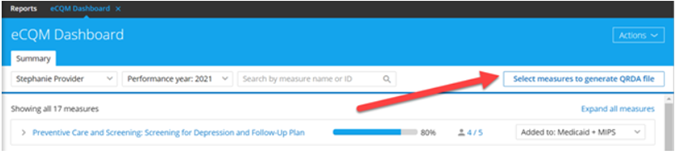
To generate a QRDA report for an individual, start by opening the eCQM Dashboard and clicking Select measures to generate QRDA file in the upper right-hand menu. A list of quality measures will open; use checkboxes to select desired eCQMs to report or click Select all measures.
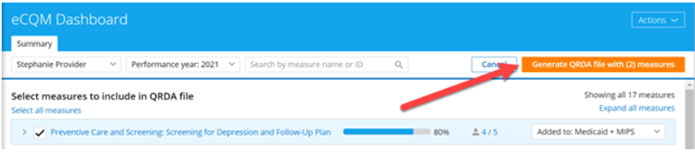
After selecting desired measures, click the orange Generate QRDA file with (X) measures button in the top menu; “X” indicates the total number of measures selected.
A detail panel will open, where you will choose the QRDA file type you wish to generate, QRDA I or QRDA III. Complete the required fields, confirming that the Tax ID number is associated with the provider listed on the QRDA file; then click Generate file. Note that file generation may take up to 24 hours. When complete, the QRDA file can be located in the Documents section of the EHR.
Group report generation
Practices participating as a group can submit quality measure data using a QRDA III. The report generation process for a group is nearly identical to generating a report for an individual.
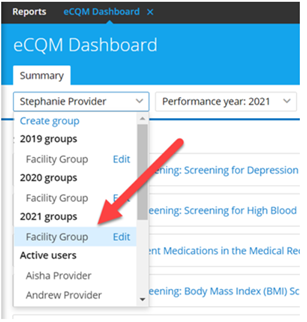
Begin by opening the eCQM Dashboard and selecting “Group” from the drop-down menu in the upper-left corner. (Note: If you do not yet have a group listed here, see How do I create a group in the eCQM Dashboard?) Select measures as described above, then click the orange Generate QRDA file with (X) measures button.
In the detail panel that opens, select the appropriate quality program: MIPS Group Reporting or MIPS Virtual Group Reporting. Complete required fields with information relevant to the Group QRDA file, specific to the selected program. The Tax ID number used should be the one associated with the group. On the next screen, confirm providers in the group and that each provider’s NPI is included; if needed, click Edit group at the top of the pane to edit providers in the group. Note that if you add providers to the group, you will need to wait up to 48 hours for calculation results to update with added providers’ information before you generate the QRDA file.
Finally, select Generate file. File generation may take up to 24 hours; when complete, the QRDA file can be located in the Documents section of the EHR.
Perform Security Risk Analysis
The Security Risk Analysis is a self-assessment required for the PI performance category score; failure to complete this analysis will result in a total score of 0 points for this performance category.
The Security Risk Analysis requirements include:
- Addressing the security (including encryption) of electronic Protected Health Information (ePHI) data that is created and/or maintained by certified electronic health record technology (CEHRT)
- Implementation of security updates as necessary
- Correctly identifying security deficiencies as part of the risk management process
The Office of the National Coordinator for Health IT (ONC) released a tool to help practices conduct and document a comprehensive security assessment to identify any risks in their organization. This tool also provides a report that is useful for required audits. Download the ONC Security Risk Analysis (SRA) Tool here.
It’s essential to keep any documentation used for your SRA in your records to prove that you completed the required Security Risk Analysis during the required time period.
Reporting this measure requires MIPS-eligible clinicians to attest YES or NO to conducting an annual self-assessment. The Security Risk Analysis must be completed before January 1, 2024.
Be prepared: 4 steps to painless MIPS reporting
Make your MIPS PY 2023 participation as painless as possible by taking time now to prepare. With 4 key actions, you can ensure your MIPS data is ready to submit, accurate, on time, and correctly formatted.
If you don’t have Practice Fusion, contact us today to learn how the Practice Fusion EHR and the MIPS Dashboard can support your MIPS goals for PY 2023 and beyond!
