June 22, 2021
Implementing ePrior authorization in your EHR workflow

Approximately 4.55 billion prescriptions were filled in 2020 and another 4.69 billion prescriptions are expected to be filled in 2021. Because of the aging population in the United States and the growing prevalence of chronic diseases, those numbers are predicted to continue growing.1 Even now, the Centers for Disease Control and Prevention (CDC) report that nearly three out of four patient visits involve drug therapy.2
A significant number of these prescription medications require prior authorization before they can be filled.
Health plans require prior authorization to make sure that patients receive medications to treat their conditions that are both appropriate and cost-effective. Health insurers require prior authorizations in certain situations, such as:3
- Brand name medications that have generic equivalents
- Expensive medications, such as specialty medications
- Medications with age limits
- Drugs identified as medically necessary by the physician, but are not covered by the health plan or pharmacy benefit manager (PBM)
- Drugs that are normally covered by the health plan or PBM, but at a lower dose than what is being prescribed
- Drugs prescribed for off-label use
Prior authorizations place a substantial burden on clinicians and their staff. The clinician and/or a staff member must request approval from the health plan or PBM by phone or fax before the prescription can be filled.4 On average, medical practices report that they must complete thirty-three prior authorizations per physician, per week.5 These prior authorizations each take an average of nearly two business days (14.4 hours) per week to complete.5 Thirty percent of physicians reported that they had staff whose exclusive responsibility was to work on gaining approval for prior authorizations. Eighty-six percent of physicians said that the burden of prior authorizations has increased over the past five years, despite efforts to simplify the process.5
Impact of prior authorizations on providers and patients
Physicians surveyed about their experience with prior authorizations overwhelmingly responded that prior authorizations often delayed patients’ access to needed care when their treatments required prior authorization.5
- 24% of physicians reported that the need for prior authorization had led to an adverse event for at least one of their patients
- 16% also said that the prior authorization process had led to a hospitalization for at least one of their patients
- 74% responded that the need for prior authorization can sometimes lead to treatment abandonment
Physicians also report that 80% of prior authorizations require extra work.6 Most physicians (64%) reported that they had to wait for at least one business day for a response to prior authorization requests from their patients’ health plans; 29% reported that they had to wait at least three business days.5 Even if the prescription was ultimately filled, 40% of prescription medications are never picked up at all, which could contribute to worsening patient health outcomes.6
Electronic prior authorizations in Practice Fusion
If you use the Practice Fusion EHR, electronic prior authorization is available whenever you prescribe a medication requiring prior authorization. This feature is automatically included in Practice Fusion, at no additional cost to licensees.4 The EHR notifies prescribers if a medication requires prior authorization as soon as they select a prescription medication, while the patient is still at the point of care. The provider can respond immediately; on average, the practice receives approval back from the prescription benefit plan or payer in about sixty seconds—enabling them to spend more time with patients.
Completing electronic prior authorization while the patient is still in the office also means that the patient can eliminate the time they would have had to spend at the pharmacy, waiting for approval for their medication to be filled. Making the process easier for patients can help improve both patient satisfaction and, ultimately, patient outcomes.4
Electronic prior authorization can also prevent unnecessary back-and-forth communication between practices, pharmacies, and health plans.7 Researchers estimate that a twenty-physician office would save approximately 1,142 staff hours a year by switching from a manual prior authorization process to electronic prior authorization.6
There are two ways to initiate an electronic prior authorization in the Practice Fusion EHR: either by sending an electronic prescription or through a manual process. In the next two sections, we walk you through both processes.
Initiate an electronic prior authorization by sending an electronic prescription
Practice Fusion streamlines the prior authorization process to make it simpler for both prescribers and patients. One way prescribers can initiate an electronic prior authorization* is by sending an electronic prescription (eRx).7
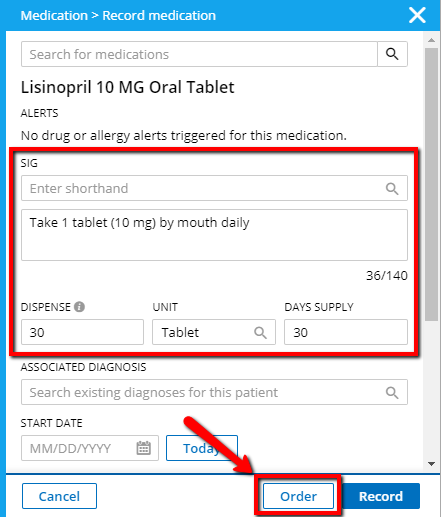
-
Choose a medication, fill in order details, then click Order.
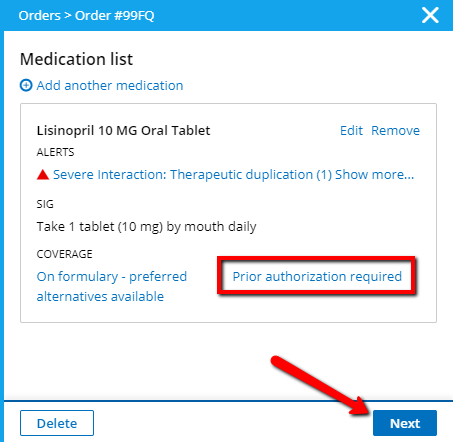
-
If the patient’s prescription benefits plan requires prior authorization for the prescribed medication to be filled, a Prior authorization required alert will display. Click Next to continue ordering the medication.
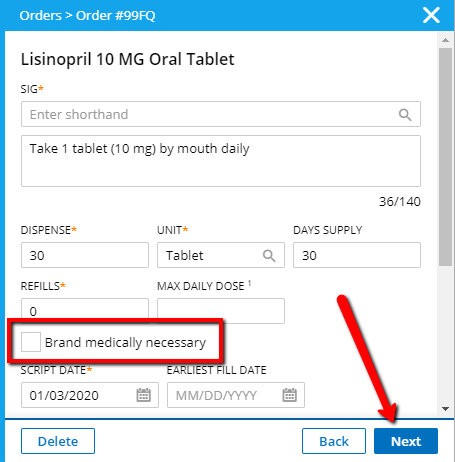
-
Review the eRx order details. If you require the originally specified brand name medication to be dispensed to the patient, mark the Brand medically necessary checkbox. If the Brand medically necessary checkbox is not selected, the pharmacy will perform a new eligibility check to determine if the patient’s prescription benefits plan requires prior authorization for the generic form of the medication. If no prior authorization is required for the generic form, the prior authorization process is not initiated.
-
Once you have reviewed the prescription details, click Next to continue the prescription medication order.
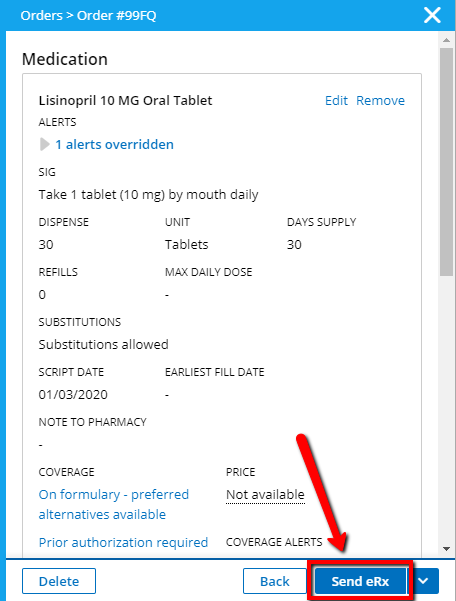
-
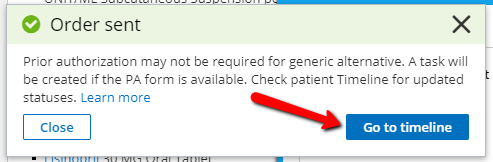
Click Send eRx to initiate the prior authorization process. Once the prescription for medication is submitted electronically, the provider will receive a notification that the prior authorization form is available, and a task has been created for completion of the form. Click Go to Timeline to check on prior authorization status.
-
The status in the patient’s Timeline for prior authorizations will be:
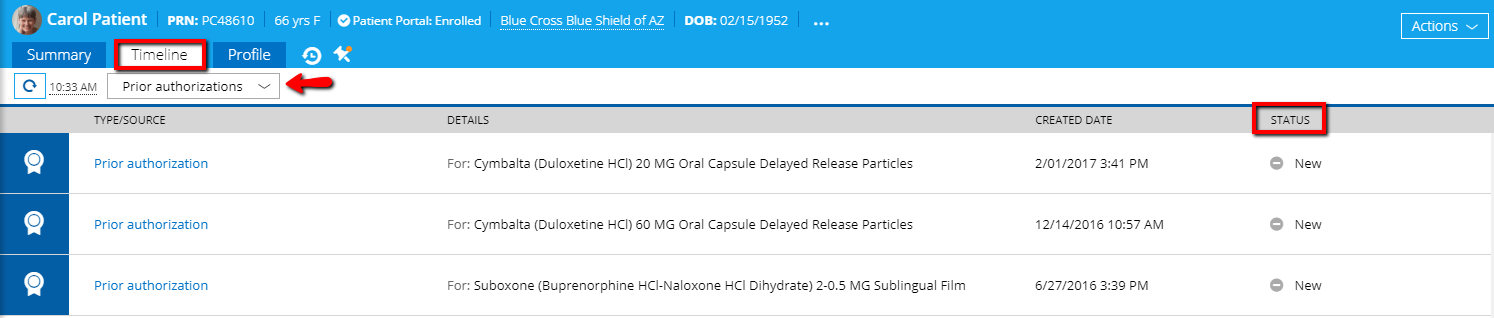
- Awaiting PA form—until you receive a question set from the payer.
- Incomplete—when you receive the form from the payer. A task is created in the Tasks section of the EHR to fill out the prior authorization form.
- Closed—if the payer did not return a question set because the patient already has a prior authorization on file or because the payer does not support electronic prior authorization.
Manually initiate an electronic prior authorization
Prescribers can also manually initiate a request for a new prior authorization by completing and submitting the required prior authorization form
First, the prescriber opens the prior authorization question set by:7
- Clicking the prior authorization labeled Incomplete in the Tasks section of the EHR, or
- Clicking the prior authorization labeled Incomplete in the patient’s Timeline, or
- Clicking the prior authorization labeled Incomplete in the patient’s Prior authorization report
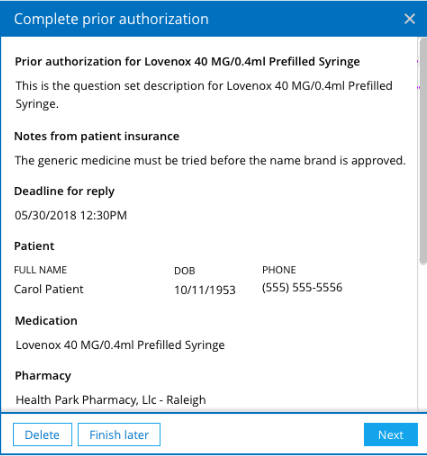
Once the question set is open, the prescriber has three choices: Click Delete to delete the form and submit a cancellation request for the prior authorization; click Finish later to complete the prior authorization question set at another time; or click Next to begin completion of the question set.7
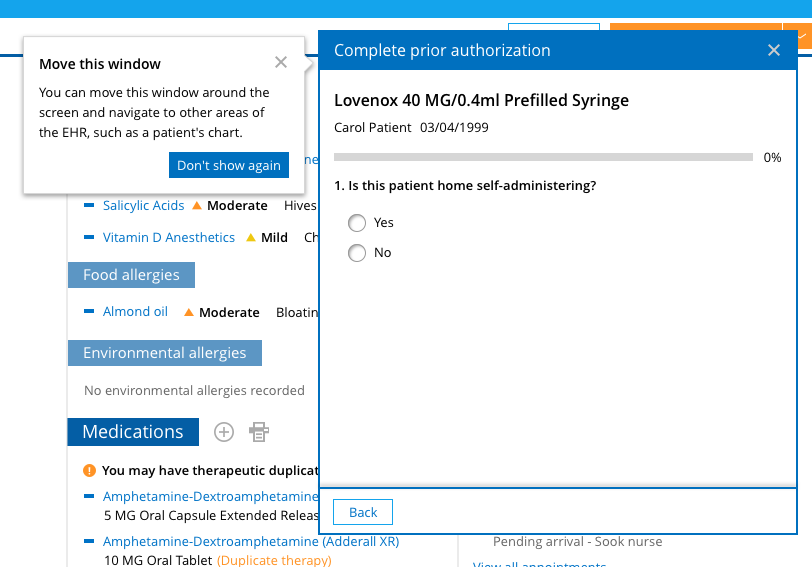
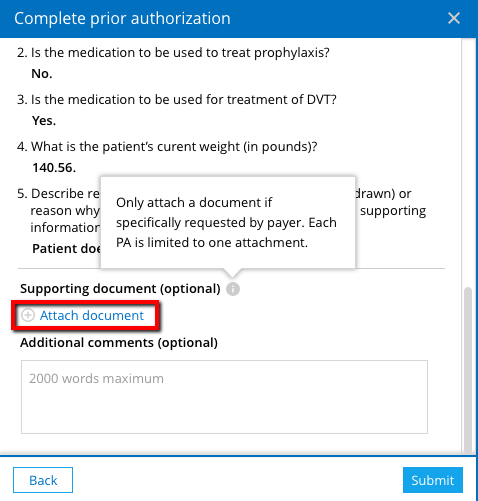
When completing the question set, note that you must answer any required question before moving to the next question on the form. For example, if a free text response is needed, the Next button will not display until you have entered text. Also, you will be able to access the patient’s chart while completing the prior authorization form. You can navigate to other areas of the EHR and the patient’s chart to help you answer questions. In addition, the question set modal can be moved around on the screen to allow you to view other windows.7
Your inputs are automatically saved while you complete the form. All your finished answers are saved even if you close the prior authorization form before completing it.
You will have the ability to attach a document at the end of the question set. Attach the document, only if it is specifically requested. You can attach only one document with a maximum size of 20 MB. Supported file types include TIFF, PNG, JPEG, PDG, CDA, and CCR.7
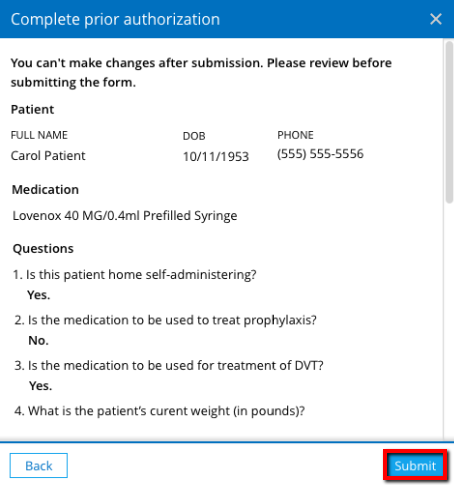
When finished completing the prior authorization form, you can review your answers before submission. You will not be able to make changes after submission. After you have reviewed your responses, click Submit to send the prior authorization question set to the payer. The prior authorization status in the Timeline and Prior authorizations report will now appear as Submitted.7
After the completed prior authorization question set is submitted, the payer will review and decide whether the patient’s benefits will cover the prescribed medication. The payer will return one of the following responses:
- Approved, indicating that the payer will cover the prescribed medication,
- Denied, indicating that the payer will not cover the prescribed medication, or
- More info needed, indicating that the payer needs additional information before making a determination
If the payer responds Approved, no further action is required. If the payer responds Denied, and the payer supports electronic appeals, the option to appeal the denial will appear in the prior authorization details. If the response is More info needed, the payer will send back an additional question set, and a task is created to complete and submit this new question set.7
Review, cancel or appeal an electronic prior authorization
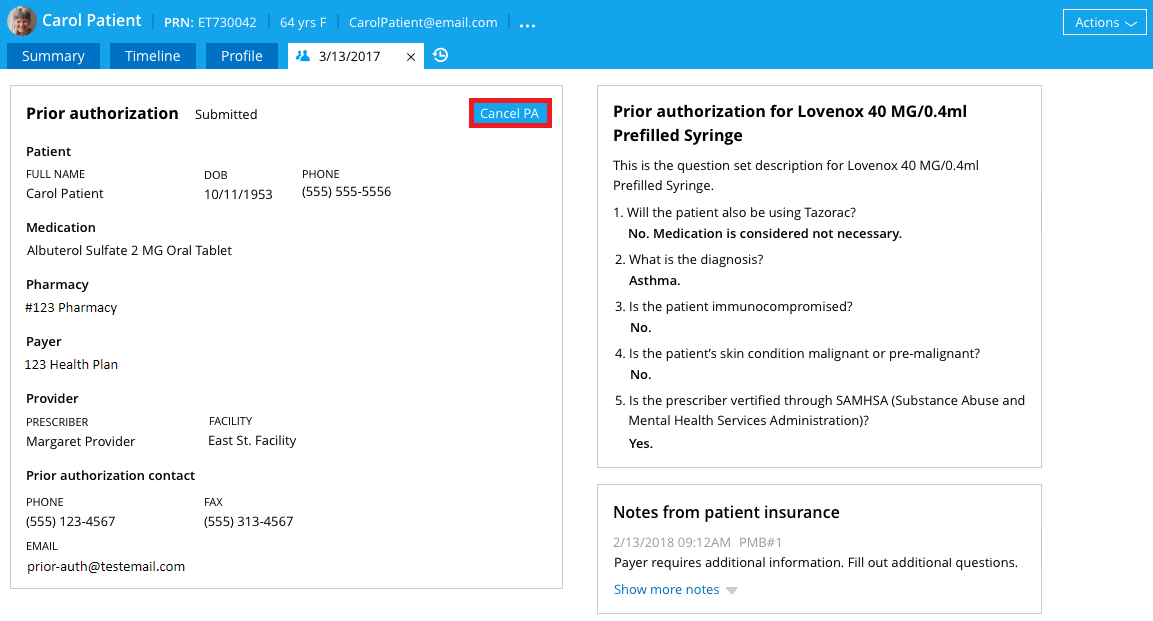
Both pending and historical prior authorizations can be accessed in the EHR, either from the Prior authorizations section of the patient Timeline or from the Prior authorizations report. In these sections of the EHR, you can also:7
- Review previously submitted forms and prior authorization notes: These can be accessed from the Details page.
- Appeal denied prior authorization: If the payer supports electronic appeals, Appeal will appear on the denied prior authorization. Click Appeal to initiate the appeal request.
- Request to cancel a prior authorization: A prior authorization can be cancelled any time after the question set is submitted, if the payer’s response is still pending. A cancellation request can be initiated from the patient’s Timeline. Click on the submitted prior authorization you wish to cancel; then click Cancel PA to send the cancellation request.
Electronic prior authorization provides formulary files to prescribers within the EHR
Formulary files are lists of prescription medications covered by the patient’s pharmacy benefit plan. With electronic prior authorization, insurers and PBMs provide these files to prescribers within the EHR to inform the prescribers about prescription medication coverage for individual patients’ pharmacy benefits.
The formulary files include formulary status for medications—which identifies whether a given drug is covered by the benefits plan—as well as alternatives. The alternatives list identifies possible alternative medications for a given medication if the PBM or insurer prefers the use of other treatment options. Coverage factors identify whether specific restrictions apply to given drugs. If a medication requires a prior authorization, the coverage factors may include this requirement.
Note that formulary data is health plan-specific, not patient-specific.8
Electronic prior authorization helps save time
Electronic prior authorization takes prior authorization from a process that eats up hours or days of staff time to a process that can often be completed in minutes.3 Practice Fusion can help handle prior authorizations for your patients’ prescriptions and allow you to make the shift from time-consuming manual prior authorizations to a more efficient, streamlined workflow.
Speeding up the prior authorization process not only can save you time, but it can also save time and reduce frustration for your patients. It can decrease the percentage of prescription medications that are never filled or abandoned at the pharmacy. It can also free up members of your practice to spend more time with patients, rather than on the phone in pursuit of prior authorizations for their prescriptions.3,5
To learn more about Practice Fusion’s electronic prior authorization feature, click here.
*Note: To effectively use electronic prior authorization, ensure that your Drug Enforcement Administration number is current and input correctly into your EHR account setting page.4
References:
- Sabanoglu T. Total number of retail prescriptions filled annually in the United States from 2013 to 2025 (in billions). Statista. Updated February 4, 2021. Accessed May 23, 2021, https://www.statista.com/statistics/261303/total-number-of-retail-prescriptions-filled-annually-in-the-us/.
- Therapeutic Drug Use. Centers for Disease Control and Prevention (CDC) Updated March 1, 2021. Accessed May 23, 2021, https://www.cdc.gov/nchs/fastats/drug-use-therapeutic.htm.
- Surescripts. Survey Results Prove Healthcare Providers Would Benefit From Electronic Prior Authorization. June 30, 2016. Accessed May 23, 2021. https://www.ahip.org/wp-content/uploads/2017/07/EPA_whitepaper-PAsurvey.pdf
- 3 Reasons Why You Need ePrior Authorization. Practice Fusion. Updated September 18, 2019. Accessed May 23, 2021, https://www.practicefusion.com/blog/reasons-implement-eprior-authorization/.
- LaPointe J. Prior Authorization Burden Continues to Rise, Physicians Report. Revcycle Intelligence. Updated June 26, 2020. Accessed May 23, 2021, https://revcycleintelligence.com/news/prior-authorization-burden-continues-to-rise-physicians-report.
- Electronic Prior Authorization webinar. Accessed May 23, 2021. https://event.on24.com/wcc/r/2122062/C4A9A43DA15DE022E9FB37E0D1CD056F?mode=login&email=cheryl.reifsnyder@allscripts.com. webinar:
- How do I use electronic prior authorization? Practice Fusion. Accessed May 22, 2021, https://help.practicefusion.com/s/article/How-do-I-use-ePrior-Authorization.
- Surescripts. Understanding Formulary & Benefits for Electronic Prior Authorization. https://go.surescripts.com/hubfs/Electronic%20Prior%20Authorization%20Tip%20Sheet%20-%20How%20Formulary%20Works.pdf
